Semiautomatically Quantified Tumor Volume Using 68Ga-PSMA-11 PET as a Biomarker for Survival in Patients with Advanced Prostate Cancer Article Swipe
 YOU?
·
· 2020
· Open Access
·
· DOI: https://doi.org/10.2967/jnumed.120.242057
· OA: W3019914727
YOU?
·
· 2020
· Open Access
·
· DOI: https://doi.org/10.2967/jnumed.120.242057
· OA: W3019914727
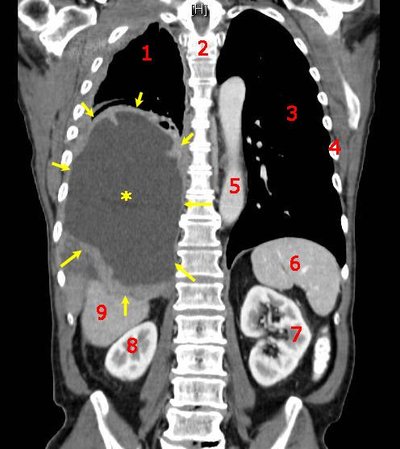
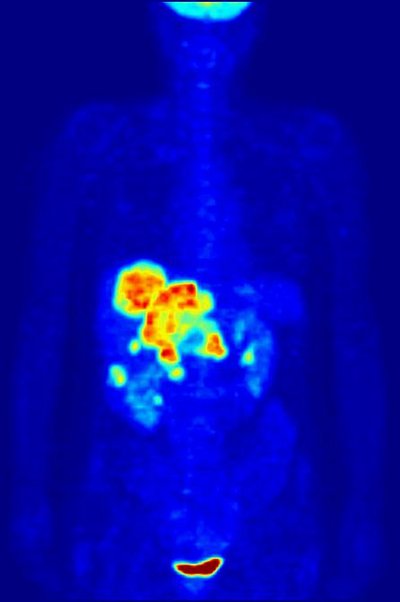
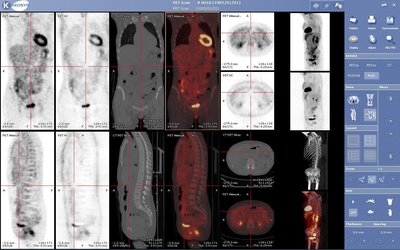
Prostate-specific membrane antigen (PSMA)-targeting PET imaging is becoming the reference standard for prostate cancer staging, especially in advanced disease. Yet, the implications of PSMA PET-derived whole-body tumor volume for overall survival are poorly elucidated to date. This might be because semiautomated quantification of whole-body tumor volume as a PSMA PET biomarker is an unmet clinical challenge. Therefore, in the present study we propose and evaluate a software that enables the semiautomated quantification of PSMA PET biomarkers such as whole-body tumor volume. <b>Methods:</b> The proposed quantification is implemented as a research prototype. PSMA-accumulating foci were automatically segmented by a percental threshold (50% of local SUV<sub>max</sub>). Neural networks were trained to segment organs in PET/CT acquisitions (training CTs: 8,632, validation CTs: 53). Thereby, PSMA foci within organs of physiologic PSMA uptake were semiautomatically excluded from the analysis. Pretherapeutic PSMA PET/CTs of 40 consecutive patients treated with <sup>177</sup>Lu-PSMA-617 were evaluated in this analysis. The whole-body tumor volume (PSMA<sub>TV50</sub>), SUV<sub>max</sub>, SUV<sub>mean</sub>, and other whole-body imaging biomarkers were calculated for each patient. Semiautomatically derived results were compared with manual readings in a subcohort (by 1 nuclear medicine physician). Additionally, an interobserver evaluation of the semiautomated approach was performed in a subcohort (by 2 nuclear medicine physicians). <b>Results:</b> Manually and semiautomatically derived PSMA metrics were highly correlated (PSMA<sub>TV50</sub>: <i>R</i><sup>2</sup> = 1.000, <i>P</i> < 0.001; SUV<sub>max</sub>: <i>R</i><sup>2</sup> = 0.988, <i>P</i> < 0.001). The interobserver agreement of the semiautomated workflow was also high (PSMA<sub>TV50</sub>: <i>R</i><sup>2</sup> = 1.000, <i>P</i> < 0.001, interclass correlation coefficient = 1.000; SUV<sub>max</sub>: <i>R</i><sup>2</sup> = 0.988, <i>P</i> < 0.001, interclass correlation coefficient = 0.997). PSMA<sub>TV50</sub> (ml) was a significant predictor of overall survival (hazard ratio: 1.004; 95% confidence interval: 1.001-1.006, <i>P</i> = 0.002) and remained so in a multivariate regression including other biomarkers (hazard ratio: 1.004; 95% confidence interval: 1.001-1.006 <i>P</i> = 0.004). <b>Conclusion:</b> PSMA<sub>TV50</sub> is a promising PSMA PET biomarker that is reproducible and easily quantified by the proposed semiautomated software. Moreover, PSMA<sub>TV50</sub> is a significant predictor of overall survival in patients with advanced prostate cancer who receive <sup>177</sup>Lu-PSMA-617 therapy.