Reply Article Swipe
 YOU?
·
· 2019
· Open Access
·
· DOI: https://doi.org/10.1002/hep4.1398
· OA: W4242501040
YOU?
·
· 2019
· Open Access
·
· DOI: https://doi.org/10.1002/hep4.1398
· OA: W4242501040
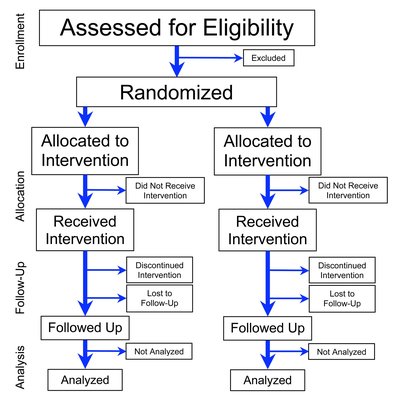
We thank Weersink and colleagues for their interest in our study and reference to available practical guidance to support medication safety in cirrhosis.1 Their recommendations are a valuable resource to assist prescribers and may reduce harm due to medication-related problems (MRPs), including “wrong drug choice,” “suboptimal dose,” and “adverse drug reactions.”2 It will be important to explore the impact of “unsafe” medications on patient outcomes in a prospective study, including the effectiveness of Weersink’s recommendations to improve medication safety. In addition to prescription of potentially inappropriate pharmacotherapy, there are several elements of a patient’s prescribed regimen that may lead to MRPs in chronic liver disease (CLD). People with decompensated cirrhosis are often required to manage a regimen that includes a variety of therapeutic classes, time-specific and medication-specific dosing instructions, and self-monitoring requirements. Additionally, changes to prescribed therapies are common due to the natural history and complications of advanced liver disease. Complex and frequently changing medication regimens can lead to confusion and affect patients’ ability to self-manage. Consequently, “safe” medications, such as diuretics and lactulose, can still be associated with harmful MRPs and hospitalization. Among the intervention patients (n = 57) enrolled in our randomized-controlled trial of pharmacist-led medication education intervention,2 over 72% of patients had ≥1 change to their medication regimen and over 22% had ≥5 changes between each intervention time point. Of these changes, 66.8% were to non-CLD therapies. The mean Medication Regimen Complexity Index (MRCI) score3 at recruitment was 25.6 ± 13.5, which is higher than a previously reported score of 20 in nonadherent pre-liver transplant patients.4 Non-CLD medications represented over three quarters of the total frequency and additional instruction complexity scores, consistent with the proportion of non-CLD medicines consumed by patients.2 While mean MRCI score did not change significantly between time points among surviving patients, those that died (n = 8) had a higher mean MRCI score at baseline (35.9 ± 18.3 vs. 23.9 ± 12.0; P = 0.019). Medication management in cirrhosis is complex, and improving medication safety requires consideration of multiple elements of a patient’s regimen from the perspective of the prescriber and the patient. We agree with Weersink and colleagues that tailored pharmacotherapy is needed to reduce unnecessary complexity and minimize use of unsafe or overprescribed medications (i.e. proton pump inhibitors) that may contribute to MRPs. There is a need for greater clinician awareness of available resources to support safe prescribing, especially outside the specialist setting given the complexity and risk for MRPs associated with non-CLD therapies.