Chronic pelvic inflammatory context leading to migraine exacerbation: a case report Article Swipe
 YOU?
·
· 2024
· Open Access
·
· DOI: https://doi.org/10.5327/cbn240363
· OA: W4416019741
YOU?
·
· 2024
· Open Access
·
· DOI: https://doi.org/10.5327/cbn240363
· OA: W4416019741
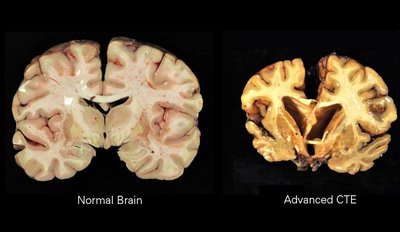
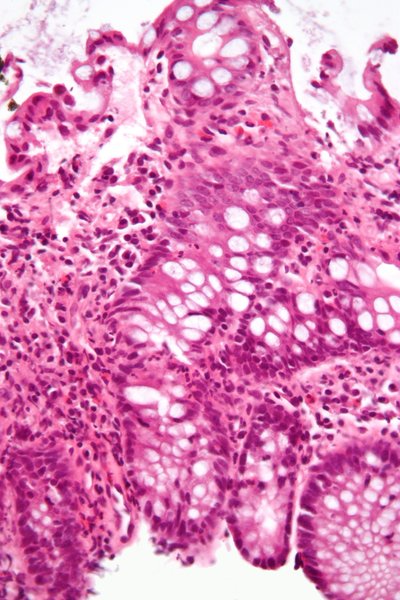
Case presentation: Woman, 48 years old, infertile, with dysmenorrhea, episodic headache since the age of 35 with weekly attacks and worsening related to the menstrual cycle. In 2020, she developed a sudden onset of dyspnea and chest pain, during menstruation which progressed to pneumothorax. A biopsy of the right upper lung lobe identified subpleural emphysema which, associated with the clinical picture of intense dysmenorrhea and magnetic resonance imaging of the pelvis, was presumptively diagnosed as a pulmonary focus of endometriosis. The patient has been menopausal since 2023 with worsening of migraine symptoms. In gynecological investigation, signs of hypoestrogenism were noted, vulvar atrophy associated with fissures in the vestibule after physical examination, cervix posterior and lateralized to the left, hypotrophic vaginal walls, shortening of the left parametrium painful upon mobilization, thickening of the endopelvic fascia and intense dysmenorrhea. After the pneumothorax, the dysmenorrhea maintained the same pattern with the headache becoming daily, located in the right temporo-occipital region, intense and pulsatile, radiating to the right hemiface with intra and extracranial allodynia, followed by progressive course, accompanied by aura with nausea, blurred vision, scotomas, photophobia and phonophobia. In the post-crisis period, there is a change in mood and hyporexia. Discussion: Endometriosis is a chronic gynecological condition characterized by the presence of endometrial tissue outside the uterus resulting in chronic pelvic pain and infertility. Endometriosis affects 60% of women and adolescents with pelvic pain and up to 50% of women with infertility. Migraine is a common neurological disorder characterized by recurrent attacks of intense headache often accompanied by nausea, vomiting and photophobia. The highest incidence occurs among women of reproductive age. A population-based study indicated that migraines are 1.7 times more common in women with endometriosis than in those without the disease, in addition to demonstrating that endometriosis is an independent predictor of migraines. One of the factors described in the literature on the pathophysiological pathways of endometriosis that may explain its apparent relationship with migraine is the activation of sensory fibers in ectopic endometrial tissue that can lead to neuronal hyperactivity throughout the central nervous system (CNS). Pulmonary manifestation demonstrates a possible exacerbation of neuronal activity in the CNS causing worsening of migraine. The scientific literature lacks prevalence rates of pulmonary endometriosis and migraines. Final comments: The role of female sex hormones in the pathogenesis of migraine is well established. The prevalence of migraine in patients with endometriosis is high and healthcare professionals need to think about both diagnostic hypotheses when caring for a patient with dysmenorrhea.
Related Topics To Compare & Contrast